A Clear Overview of Ductal Carcinoma and How It’s Diagnosed
Ductal carcinoma develops in the milk ducts and is commonly detected through screenings, imaging, and biopsies. Understanding the typical characteristics, risk factors, and diagnostic approaches offers educational insight while remaining strictly neutral, not implying personal diagnosis, treatment guidance, or guaranteed outcomes.

Ductal carcinoma begins in the milk ducts of the breast and includes two broad categories: noninvasive disease that stays inside the ducts and invasive disease that grows beyond them. Understanding these terms helps make sense of screening results and medical recommendations. While many people first learn about ductal carcinoma through a routine mammogram, some notice physical changes like a new lump or nipple changes. Diagnosis typically combines imaging and a biopsy, and the final pathology report guides next steps.
Understanding what ductal carcinoma is
Ductal carcinoma refers to cancers that start in the cells lining the milk ducts, the tiny channels that carry milk to the nipple. It is distinct from lobular carcinoma, which arises in the milk-producing lobules. When doctors evaluate ductal tumors, they assess how the cells look under a microscope, whether they have hormone receptors, and how fast they appear to be growing. These details help characterize the disease and inform treatment planning later on. Although the focus here is on what it is and how it is found, recognizing that ductal cancers vary in behavior and biology is important for understanding clinical decisions.
DCIS vs invasive ductal carcinoma
Differences between DCIS and invasive ductal carcinoma matter because they reflect whether cancer cells have moved beyond the duct. Ductal carcinoma in situ, or DCIS, is considered noninvasive or stage 0 because the abnormal cells remain inside the ducts. DCIS can be low, intermediate, or high grade and is often detected on screening mammograms as clusters of tiny calcifications. Invasive ductal carcinoma, sometimes called IDC, has broken through the duct wall and can grow into surrounding breast tissue, with the potential to reach lymph nodes or travel elsewhere. Staging for invasive disease considers tumor size, lymph node involvement, and other factors. Pathology reports for both DCIS and invasive cancer typically include receptor status such as estrogen and progesterone receptors and HER2, which helps guide therapy planning.
Common symptoms linked to ductal carcinoma
Common symptoms linked to ductal carcinoma include a new breast lump or thickening, a change in the size or shape of the breast, dimpling or puckering of the skin, redness or scaling of the nipple or breast skin, nipple inversion that is new, and nipple discharge that may be clear or bloody. Pain is not a reliable indicator by itself, as many breast cancers are painless, and many painful lumps are benign. Importantly, many people have no noticeable symptoms, and ductal carcinoma is found on routine screening mammograms before a lump can be felt. Men can also develop ductal carcinoma, though it is less common, and symptoms may mirror those in women. Any new, persistent change warrants evaluation to determine the cause.
How ductal carcinoma is diagnosed
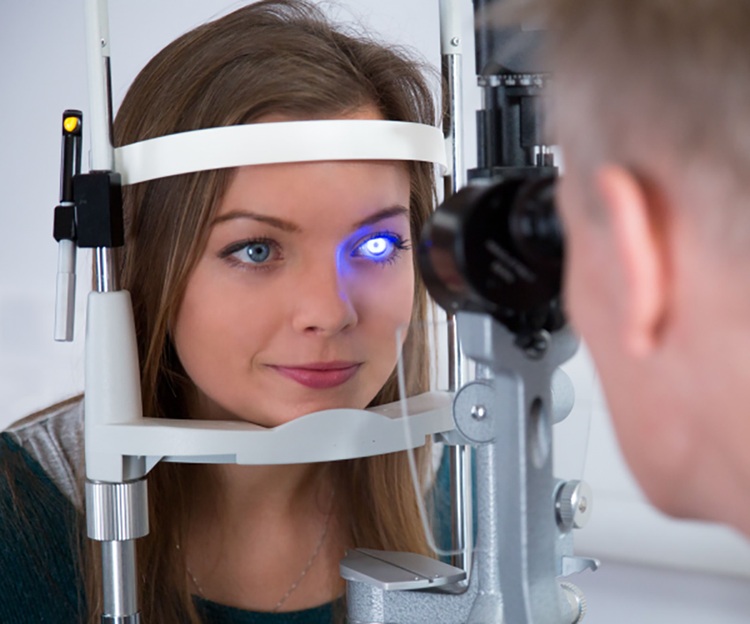
How ductal carcinoma is diagnosed usually starts with imaging. Screening mammography is used for people without symptoms, and if something unusual is seen, diagnostic mammography provides additional, focused views. Breast ultrasound is commonly added to evaluate a finding seen on mammography or to assess a palpable area. Breast MRI may be recommended for people with very dense breasts, higher inherited risk, or when images are difficult to interpret. If imaging suggests an area of concern, the next step is a needle biopsy. Core needle biopsy, performed under imaging guidance such as ultrasound, mammography, or MRI, removes small tissue samples for a pathologist to examine. The pathology report confirms whether the finding is DCIS or invasive, assigns a grade, and tests for hormone receptors and HER2. For invasive cancers, imaging or surgical evaluation of nearby lymph nodes may be advised. Some individuals may be referred for genetic counseling and testing, particularly when there is a strong family history or an early age at diagnosis. Local services in your area typically coordinate these steps so results flow into a clear plan.
Interpreting imaging and pathology results
Mammogram findings are often described using a standardized scale that indicates the level of concern and the recommended next action, such as short interval follow up imaging or biopsy. Ultrasound can differentiate solid from fluid filled areas and guide precise biopsy. When the biopsy is complete, the pathology report becomes the central document. It notes whether the cells are confined inside the ducts or have invaded surrounding tissue, the grade that reflects how abnormal and fast growing the cells appear, and receptor status that signals whether growth may be driven by hormones or by HER2. While these details can be technical, they explain why two people with ductal carcinoma might receive different recommendations. High quality communication with the care team can help translate these terms into a clear understanding.
What to expect after a diagnosis
After a confirmed diagnosis, clinicians consider overall health, tumor characteristics, and personal preferences to outline options. For DCIS, choices may differ from those for invasive disease because the biology and risks are not the same. Additional imaging, surgical consultation, or discussions about systemic therapies may be part of planning. Not every test is needed for every person; the aim is to answer specific questions that influence safety and effectiveness. People who live far from large centers can usually complete core steps using local services, with specialized input added as needed. Keeping copies of imaging reports and pathology summaries helps ensure continuity as appointments progress.
Conclusion A clear understanding of ductal carcinoma starts with knowing where it begins in the breast and whether it is confined to the ducts or has become invasive. Recognizing common symptoms, the role of screening, and the importance of biopsy and pathology helps make sense of next steps. With a structured diagnostic process and clear communication, most people can move from uncertainty to a well defined plan tailored to their situation.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.