CAR T-Cell Therapy: An Innovative Approach to Cancer Treatment
CAR‑T treatments for cancer use modified immune cells to target certain cancer types. Learning about how the therapy works, possible effects, and guidance from healthcare professionals can help patients understand this approach as part of broader treatment options without promising specific outcomes.
Understanding the Benefits of CAR T Treatments for Cancer
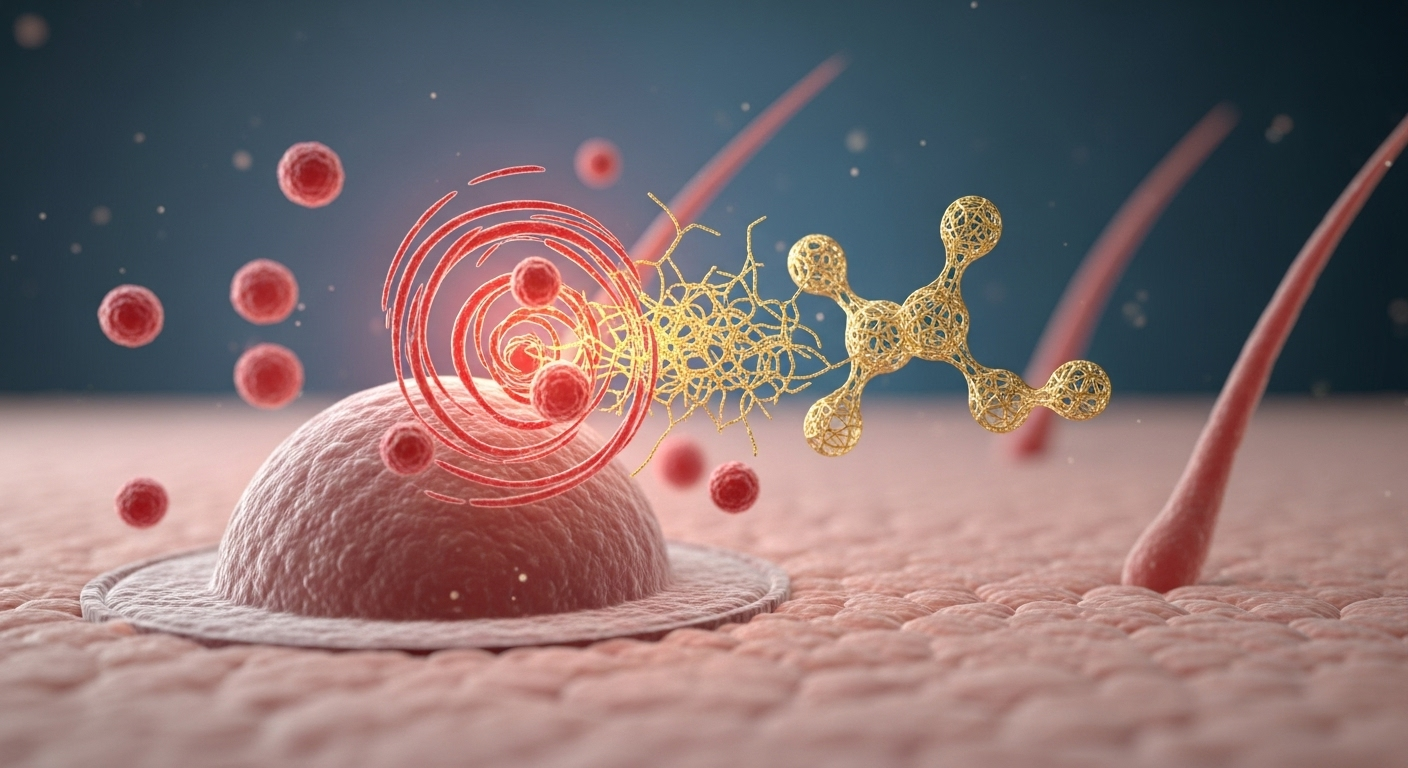
CAR T-cell therapy (Chimeric Antigen Receptor T-cell therapy) works by enhancing the natural cancer-fighting abilities of the immune system. Unlike conventional cancer treatments that directly attack cancer cells, CAR T therapy reprograms the patient’s own T cells to recognize and eliminate cancer cells throughout the body. This approach offers several significant benefits over traditional cancer treatments.
One of the primary advantages is the potential for durable remissions in patients with certain blood cancers who have exhausted other treatment options. Clinical trials have shown remarkable response rates, with some patients experiencing complete remission that lasts for years. Additionally, CAR T therapy is typically administered as a single infusion, unlike chemotherapy which often requires multiple cycles over months. This one-time treatment approach can significantly reduce the time patients spend in treatment facilities.
Another benefit is the systemic nature of the therapy. Once the modified T cells are in the bloodstream, they can travel throughout the body, potentially reaching cancer cells in multiple locations. This makes CAR T therapy particularly valuable for addressing metastatic disease or cancer that has spread beyond its original site.
How CAR T Therapy Works for Cancer Treatment
The CAR T treatment process begins with collecting T cells from the patient’s blood through a procedure called leukapheresis. This process separates and collects white blood cells, including T cells, while returning the remaining blood components to the patient. The collected T cells are then sent to a specialized laboratory where they undergo genetic modification.
In the laboratory, scientists use viral vectors to insert genetic instructions that enable the T cells to produce chimeric antigen receptors (CARs) on their surface. These receptors are specifically designed to recognize proteins (antigens) found on the surface of cancer cells. After modification, the engineered T cells are multiplied in the laboratory until they number in the millions.
Before receiving the modified T cells, patients typically undergo a brief course of chemotherapy known as lymphodepletion. This preparatory step helps create space for the new CAR T cells and improves their chances of multiplying and persisting in the body. The engineered CAR T cells are then infused back into the patient’s bloodstream, where they begin their cancer-fighting mission by seeking out and destroying cancer cells that display the target antigen.
CAR T Treatment Eligibility for Cancer Patients
Currently, CAR T-cell therapy is FDA-approved for specific types of blood cancers, including certain forms of leukemia, lymphoma, and multiple myeloma. Patients typically become eligible for CAR T therapy after trying and not responding adequately to at least two previous lines of treatment, making it primarily a third-line or later treatment option.
For B-cell acute lymphoblastic leukemia (ALL), eligibility is generally limited to patients up to age 25 who have relapsed or refractory disease. For diffuse large B-cell lymphoma (DLBCL), follicular lymphoma, and mantle cell lymphoma, adult patients who have failed previous treatments may qualify. Multiple myeloma patients who have received at least four prior lines of therapy may also be eligible for specific CAR T products targeting the BCMA antigen.
Several factors influence patient selection for CAR T therapy. Medical teams evaluate a patient’s overall health status, organ function, and ability to withstand potential side effects. Age alone is not necessarily a limiting factor, though older patients must have adequate organ function and performance status. The presence of certain medical conditions, particularly those affecting the heart, lungs, kidneys, or neurological system, may impact eligibility due to the risk of severe side effects.
Managing Side Effects of CAR T-Cell Therapy
While CAR T therapy offers remarkable benefits, it can also cause significant side effects that require careful monitoring and management. The most common serious side effect is cytokine release syndrome (CRS), which occurs when the activated T cells release large amounts of inflammatory molecules called cytokines. CRS can cause symptoms ranging from mild flu-like conditions to severe inflammatory responses requiring intensive care.
Another potential complication is neurotoxicity, now termed immune effector cell-associated neurotoxicity syndrome (ICANS). This can manifest as confusion, difficulty speaking, seizures, or other neurological symptoms. Both CRS and ICANS typically occur within days to weeks after CAR T-cell infusion and are usually temporary and reversible with proper medical intervention.
Treatment centers administering CAR T therapy must have specialized expertise in managing these unique side effects. The FDA requires that centers offering commercial CAR T products be certified to ensure they have the necessary protocols, training, and equipment to safely administer these therapies and manage potential complications. Medications such as tocilizumab (an IL-6 receptor antagonist) and corticosteroids are commonly used to control severe CRS and ICANS.
The Future of CAR T Therapy in Cancer Treatment
The field of CAR T therapy is rapidly evolving, with researchers exploring ways to expand its applications beyond blood cancers to solid tumors such as breast, lung, and pancreatic cancer. This represents one of the most significant challenges and opportunities in the field, as solid tumors present unique barriers including physical obstacles that prevent T-cell infiltration and immunosuppressive tumor microenvironments.
Scientists are developing next-generation CAR T cells with enhanced capabilities, such as the ability to target multiple cancer antigens simultaneously, overcome immunosuppressive factors, or include safety switches that can deactivate the cells if severe side effects occur. “Off-the-shelf” allogeneic CAR T cells derived from healthy donors rather than individual patients may eventually make treatment more accessible and reduce production time and costs.
Clinical trials are also investigating CAR T therapy as an earlier line of treatment rather than waiting until patients have exhausted multiple other options. Early results suggest that using these therapies earlier in the disease course might lead to better outcomes with fewer side effects, potentially changing the standard approach to treating certain cancers in the future.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




