Diabetes Treatment Through Self-Care and Lifestyle Management
Diabetes self-care solutions focus on daily habits that help manage blood sugar and overall health. These include monitoring glucose levels, following a balanced diet, staying active, and taking medications as prescribed. Consistent self-care supports better control and reduces the risk of complications.
How to Manage Diabetes With Self-Care Practices
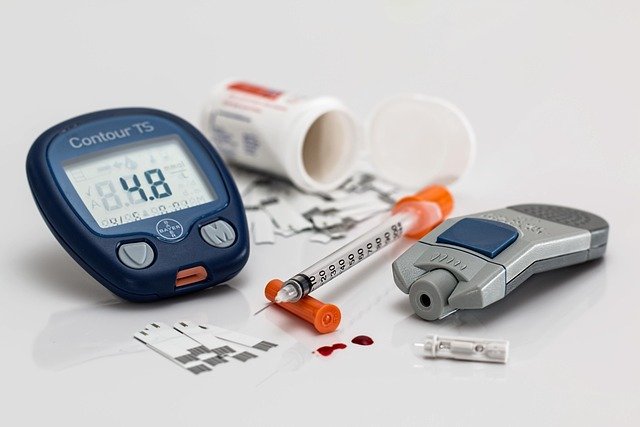
Self-care practices form the foundation of successful diabetes management, encompassing daily activities that directly impact blood glucose control. Blood glucose monitoring stands as the most fundamental self-care practice, requiring individuals to check their levels multiple times daily using a glucose meter or continuous glucose monitor. This routine provides valuable data that guides medication timing, meal planning, and activity levels.
Medication adherence represents another critical self-care component. Whether managing Type 1 diabetes with insulin injections or Type 2 diabetes with oral medications, consistent timing and proper dosing ensure optimal blood sugar control. Many individuals benefit from using pill organizers, smartphone apps, or alarm systems to maintain their medication schedule.
Foot care deserves special attention in diabetes self-care routines. Daily foot inspections, proper wound care, and appropriate footwear selection help prevent serious complications like diabetic foot ulcers. Regular dental care also plays a vital role, as diabetes increases the risk of gum disease and other oral health issues.
How Lifestyle Changes Support Diabetes Self-Care
Lifestyle modifications create the environmental conditions necessary for effective diabetes self-care practices to flourish. Sleep quality significantly impacts blood sugar regulation, with inadequate rest leading to insulin resistance and elevated glucose levels. Establishing consistent sleep schedules and creating optimal sleep environments support better diabetes management outcomes.
Stress management techniques complement medical treatments by addressing cortisol-related blood sugar spikes. Regular practice of relaxation methods, meditation, or yoga helps maintain emotional balance while supporting physical health. Many individuals find that stress reduction techniques improve their ability to maintain other self-care practices consistently.
Social support systems enhance lifestyle change sustainability. Connecting with diabetes support groups, working with certified diabetes educators, or involving family members in management routines creates accountability and encouragement. Educational resources and continuous learning about diabetes management empower individuals to make informed decisions about their health.
Managing Diabetes Through Lifestyle and Nutrition
Nutritional management serves as a cornerstone of diabetes treatment, requiring understanding of how different foods affect blood glucose levels. Carbohydrate counting enables precise insulin dosing for those using insulin, while consistent meal timing helps maintain stable blood sugar patterns throughout the day. Working with registered dietitians familiar with diabetes management provides personalized guidance for creating sustainable eating plans.
Physical activity offers multiple benefits for diabetes management, improving insulin sensitivity and glucose uptake by muscles. Regular exercise routines that combine cardiovascular activities with resistance training provide optimal results. However, individuals must learn to adjust medication and monitor blood glucose before, during, and after exercise to prevent dangerous fluctuations.
Portion control and meal planning strategies help maintain consistent carbohydrate intake while ensuring nutritional adequacy. Many successful diabetes managers prepare meals in advance, use measuring tools, and keep detailed food logs to identify patterns between eating habits and blood glucose responses.
Understanding Treatment Costs and Healthcare Options
Diabetes treatment expenses vary significantly based on insurance coverage, medication types, and monitoring technology preferences. Monthly costs typically range from $200 to $500 for individuals with insurance, while uninsured individuals may face expenses exceeding $1,000 monthly.
| Treatment Component | Monthly Cost Range | Insurance Coverage |
|---|---|---|
| Glucose Test Strips | $50-$150 | Usually covered |
| Insulin (Type 1) | $100-$300 | Varies by plan |
| Oral Medications | $30-$200 | Generic often covered |
| Continuous Glucose Monitor | $150-$350 | Increasingly covered |
| Medical Appointments | $200-$400 | Copay dependent |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
Various assistance programs help reduce diabetes treatment costs. Pharmaceutical companies offer patient assistance programs for qualifying individuals, while community health centers provide sliding-scale fee structures. State programs and nonprofit organizations also provide resources for diabetes supplies and education.
Long-term Success Strategies
Sustainable diabetes management requires developing routines that integrate seamlessly with daily life. Successful individuals often emphasize the importance of flexibility within structure, allowing for adjustments while maintaining core self-care practices. Regular healthcare team communication ensures treatment plans evolve with changing needs and circumstances.
Technology integration supports long-term adherence through smartphone apps that track blood glucose, medication reminders, and food logging capabilities. Many modern glucose monitors sync with mobile devices, creating comprehensive data records that inform treatment decisions.
Building diabetes management skills gradually prevents overwhelm while ensuring comprehensive care. Starting with basic practices and progressively adding more sophisticated management techniques creates sustainable habits that support long-term health outcomes.
Effective diabetes treatment combines medical interventions with comprehensive self-care practices and lifestyle modifications. Success depends on consistent implementation of monitoring routines, nutritional strategies, physical activity, and stress management techniques. While treatment costs present challenges, various resources and assistance programs help make diabetes care more accessible. The integration of technology, healthcare team support, and personal commitment creates the framework for successful long-term diabetes management and improved quality of life.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




