Understanding Plasma Therapy and Its Applications
Plasma therapy involves using components of blood plasma for various medical and therapeutic applications. It may be used in contexts such as wound healing, recovery support, and research settings. Understanding these general applications provides a neutral perspective on how plasma therapy is utilized without implying specific outcomes.
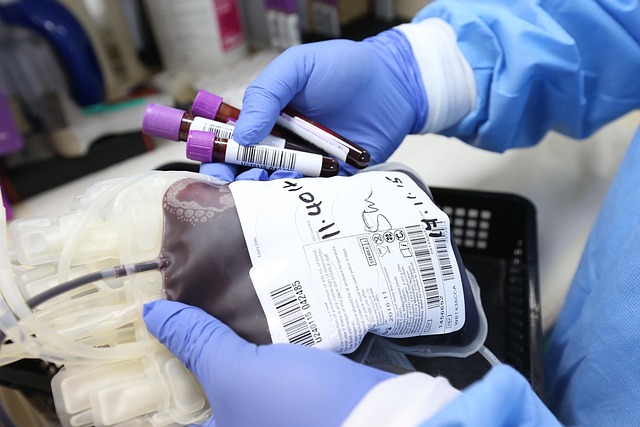
Plasma therapy represents a cornerstone of modern medicine, utilizing the liquid component of blood that contains essential proteins, antibodies, and clotting factors. Medical professionals have employed this treatment modality for decades, continuously expanding its applications as research reveals new therapeutic possibilities. The process involves separating plasma from whole blood and administering it to patients who lack specific blood components or require immune system support.
Understanding Plasma Therapy and Its Uses
Plasma therapy encompasses several distinct treatment approaches, each designed to address specific medical needs. The most common form involves transfusing fresh frozen plasma to patients experiencing severe bleeding or clotting disorders. This treatment provides critical clotting factors that help control hemorrhaging during surgeries or traumatic injuries. Another widely used application is immunoglobulin therapy, where concentrated antibodies extracted from plasma help patients with weakened immune systems fight infections. Plasmapheresis, a therapeutic plasma exchange procedure, removes harmful substances from the bloodstream while replacing the plasma with donor plasma or a plasma substitute. This technique proves particularly valuable for treating autoimmune conditions where the body produces antibodies that attack its own tissues.
Convalescent plasma therapy gained significant attention during recent global health challenges, as it involves collecting plasma from recovered patients who have developed antibodies against specific infections. Medical facilities administer this antibody-rich plasma to individuals currently fighting the same infection, potentially reducing symptom severity and recovery time. Albumin therapy, another plasma-derived treatment, addresses conditions causing low protein levels in the blood, including liver disease and severe burns.
Overview of Common Applications of Plasma Therapy
The medical community employs plasma therapy across numerous specialties and conditions. Hematology departments frequently use plasma transfusions for patients with hemophilia, von Willebrand disease, and other inherited bleeding disorders. These individuals lack specific clotting factors naturally present in plasma, making regular infusions essential for preventing dangerous bleeding episodes. Trauma centers rely heavily on plasma therapy when treating patients with massive blood loss, as rapid plasma administration can mean the difference between life and death.
Neurology departments utilize plasma exchange therapy for patients with Guillain-Barré syndrome, myasthenia gravis, and chronic inflammatory demyelinating polyneuropathy. These autoimmune neurological conditions respond well to removing harmful antibodies from the bloodstream. Rheumatology specialists employ similar techniques for treating severe cases of lupus and other systemic autoimmune diseases. Oncology centers incorporate plasma-derived immunoglobulins into treatment protocols for patients whose cancer treatments have compromised their immune systems.
Burn units depend on albumin therapy to maintain proper fluid balance and protein levels in patients with extensive burns. The liver disease treatment landscape includes plasma exchange as a bridge therapy for patients awaiting transplants or experiencing acute liver failure. Infectious disease specialists continue exploring convalescent plasma applications for emerging viral infections, building on decades of experience using this approach during various outbreaks.
Understanding How Plasma Therapy Fits Into Modern Treatments
Contemporary medicine integrates plasma therapy into comprehensive treatment plans rather than using it as a standalone solution. Physicians carefully evaluate each patient’s condition, medical history, and specific needs before recommending plasma-based interventions. The therapy often works alongside other treatments, including medications, surgery, and supportive care measures. Advanced medical centers employ sophisticated protocols to ensure plasma compatibility and minimize adverse reactions.
Modern plasma therapy benefits from technological improvements in collection, processing, and storage methods. Automated apheresis machines allow precise separation of plasma components, maximizing therapeutic effectiveness while minimizing donor discomfort. Rigorous screening procedures ensure plasma safety, with multiple tests performed to detect infectious diseases and other potential contaminants. Specialized freezing and storage techniques preserve plasma quality for extended periods, enabling blood banks to maintain adequate supplies for emergency situations.
Research institutions continuously investigate new applications for plasma therapy, exploring its potential in regenerative medicine, wound healing, and tissue repair. Clinical trials examine whether plasma-derived growth factors can accelerate recovery from injuries or improve outcomes in degenerative conditions. The scientific community also studies optimal dosing strategies, treatment timing, and patient selection criteria to enhance therapeutic results.
Healthcare providers emphasize that plasma therapy success depends on proper patient selection and careful monitoring throughout treatment. Medical teams assess potential risks against expected benefits, considering factors such as the patient’s overall health status, the severity of their condition, and available alternative treatments. Regular follow-up appointments allow physicians to evaluate treatment effectiveness and adjust protocols as needed.
The integration of plasma therapy into modern medical practice reflects a broader trend toward personalized medicine, where treatments are tailored to individual patient characteristics and needs. As understanding of plasma components deepens and technology advances, the scope of plasma therapy applications continues expanding, offering new possibilities for managing previously challenging medical conditions.
Conclusion
Plasma therapy stands as a vital component of contemporary medical treatment, offering solutions for diverse conditions ranging from bleeding disorders to autoimmune diseases. Its versatility and proven effectiveness have secured its place in hospitals and treatment centers worldwide. As research progresses and technology evolves, plasma therapy will likely expand its role in healthcare, providing hope and healing to patients facing serious medical challenges. The continued development of plasma-based treatments demonstrates medicine’s commitment to harnessing natural biological resources to improve patient outcomes and quality of life.