Understanding the Recovery Process After Cataract Surgery
Recovery from cataract surgery often involves rest, eye protection, and gradual adaptation to improved vision. Understanding the typical steps and expected experiences provides educational insight without implying guaranteed outcomes, promoting specific surgeons, or offering personal medical advice.

This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
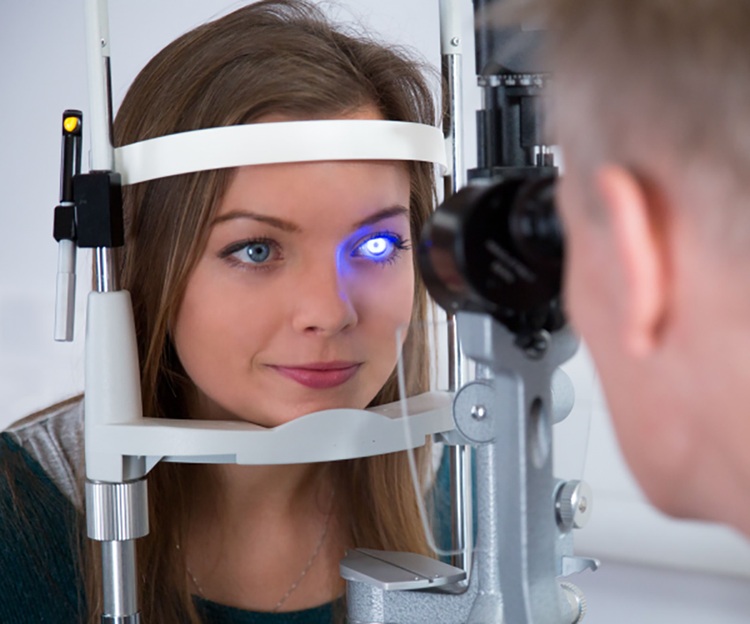
Cataract surgery involves replacing the eye’s clouded natural lens with an artificial intraocular lens (IOL). While the procedure is typically performed on an outpatient basis, the recovery phase is a critical period where the eye heals and adapts to the new lens. Patients are usually monitored for a short time immediately after the surgery before being allowed to go home with specific instructions. Adhering to these post-operative guidelines is essential for a smooth and effective recovery, helping to minimize complications and ensure successful vision restoration.
What to Expect During Cataract Surgery Recovery?
Immediately after cataract surgery, it is common to experience some mild discomfort, such as itching, a gritty sensation, or slight redness in the eye. These symptoms are generally temporary and can often be managed with prescribed eye drops and over-the-counter pain relievers if recommended by a healthcare professional. It is important to avoid rubbing or applying pressure to the treated eye. A protective shield or patch may be advised, especially during sleep, to prevent accidental contact. Many people notice an improvement in their vision almost immediately, though it may initially appear blurry, wavy, or distorted as the eye adjusts to the new lens and resolves any residual swelling. Sensitivity to light is also a frequent initial experience.
Patients will typically receive detailed instructions regarding activities to avoid during the initial recovery period. These often include refraining from strenuous activities, heavy lifting, bending at the waist, and swimming. It is also usually recommended to avoid getting water directly into the eye when showering or washing hair. Follow-up appointments are scheduled to monitor the healing process, check the eye’s pressure, and ensure there are no signs of infection or complications. The consistent use of prescribed medicated eye drops, which typically include antibiotics and anti-inflammatory agents, is vital to prevent infection and control inflammation.
What is the Typical Healing Timeline After Cataract Surgery?
The healing timeline after cataract surgery varies from person to person, but there is a general progression that most individuals follow. In the first few days post-surgery, vision may fluctuate, and the eye might feel sensitive. Most significant discomfort usually subsides within 24 to 48 hours. By the end of the first week, many patients report substantial improvements in their vision, with less blurriness and increased clarity. However, some minor residual blurriness or light sensitivity can still be present. Regular use of prescribed eye drops continues to be a key part of this initial phase.
Over the next few weeks, typically within one month, the eye continues to heal, and vision stabilizes further. Most restrictions on daily activities are gradually lifted as advised by the ophthalmologist. It is common for the final visual acuity to be assessed around four to six weeks post-surgery. While the majority of healing occurs within the first few weeks, complete recovery and vision optimization can take several months as the brain fully adapts to the new lens and improved visual input. For patients undergoing surgery on both eyes, there is usually a waiting period of several weeks between procedures to allow the first eye to heal completely.
How Do Vision Changes Manifest During Recovery?
Vision changes during recovery from cataract surgery can be quite noticeable and often progress positively. Immediately after the procedure, it is common for vision to be blurry or hazy. This is often due to residual effects of the anesthetic, temporary swelling, or the eye adjusting to the new intraocular lens. Colors may appear brighter or have a different hue than before, a phenomenon attributed to the removal of the yellowed cataract that had filtered light entering the eye. This enhanced color perception typically normalizes as the brain adapts.
Some individuals might experience glare or halos around lights, especially at night. This can be a temporary effect of the new IOL or part of the eye’s adjustment process. For most, these visual disturbances diminish over time, though some may persist depending on the type of IOL implanted. Near vision may also take longer to fully settle, particularly if a monofocal lens was chosen, which means glasses might still be required for reading or specific tasks. Regular follow-up appointments allow the ophthalmologist to monitor these changes and provide guidance on when vision correction, such as new glasses, might be beneficial to achieve the best possible outcome.
Recovering from cataract surgery is a journey that involves careful adherence to post-operative instructions and patience. While significant improvements in vision are often experienced quickly, the full benefits of the surgery unfold gradually over weeks and months. Understanding the typical expectations for discomfort, activity restrictions, and visual changes can help individuals prepare for and navigate this important healing period effectively, leading to restored clarity and an improved quality of life.